-Aarfai
Brain LLLT
Recently, Longecity member LongLife asked about the transcranial low level laser therapy wavelengths that have been tested in humans for brain enhancement, traumatic brain injury recovery, stroke, etc.

So, I figured I would make a page that lists all of the wavelengths that have been tested in the scientific literature on human brains.
As most of you will remember, a wavelength is the distance from crest to crest and is one of the most important parameters of low level laser therapy (LLLT).

The ‘nm’ stands for nanometers.
There are one billion nanometers in one meter.

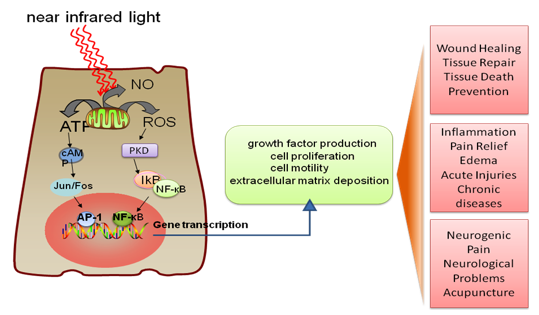
The typical wavelengths of light used in LLLT for brain enhancement are in the near infrared range (approx. 700 nm to 2500 nm).


So far, 808/810, 870, and 1064 nm have been the most common transcranial LLLT wavelengths in the human studies because they penetrate deeply and stimulate mitochondria in the brain.

Without further ado, here are the transcranial LLLT wavelengths that have been tested on humans!
Wavelengths
1064 nm R
1064 nm R
1064 nm R
810 and 980 nm R
810 and 980 nm R
1064 nm R
627 nm R
870 and 633 nm R
1064 nm R
870 and 633 nm R
810 nm R
808 nm R
808 nm R
Devices I Use and Where To Purchase
850 nm 96 LED Array
850 nm 48 LED Array + Adapter
810 nm Vetrolaser
660 nm Tendlite
The Studies
https://www.ncbi.nlm.nih.gov/pubmed/27267860
Brain Stimul. 2016 May 24. pii: S1935-861X(16)30105-X. doi: 10.1016/j.brs.2016.05.009. [Epub ahead of print]
Transcranial Laser Stimulation as Neuroenhancement for Attention Bias Modification in Adults with Elevated Depression Symptoms.
Disner SG1, Beevers CG2, Gonzalez-Lima F3.
Author information
Abstract
BACKGROUND:
Low-level light therapy (LLLT) with transcranial laser is a non-invasive form of neuroenhancement shown to regulate neuronal metabolism and cognition. Attention bias modification (ABM) is a cognitive intervention designed to improve depression by decreasing negative attentional bias, but to date its efficacy has been inconclusive. Adjunctive neuroenhancement to augment clinical effectiveness has shown promise, particularly for individuals who respond positively to the primary intervention.
OBJECTIVE/HYPOTHESIS:
This randomized, sham-controlled proof-of-principle study is the first to test the hypothesis that augmentative LLLT will improve the effects of ABM among adults with elevated symptoms of depression.
METHODS:
Fifty-one adult participants with elevated symptoms of depression received ABM before and after laser stimulation and were randomized to one of three conditions: right forehead, left forehead, or sham. Participants repeated LLLT two days later and were assessed for depression symptoms one and two weeks later.
RESULTS:
A significant three-way interaction between LLLT condition, ABM response, and time indicated that right LLLT led to greater symptom improvement among participants whose attention was responsive to ABM (i.e., attention was directed away from negative stimuli). Minimal change in depression was observed in the left and sham LLLT.
CONCLUSIONS:
The beneficial effects of ABM on depression symptoms may be enhanced when paired with adjunctive interventions such as right prefrontal LLLT; however, cognitive response to ABM likely moderates the impact of neuroenhancement. The results suggest that larger clinical trials examining the efficacy of using photoneuromodulation to augment cognitive training are warranted.
https://www.ncbi.nlm.nih.gov/pubmed/27220529
Lasers Med Sci. 2016 May 25. [Epub ahead of print]
Cognitive enhancement by transcranial laser stimulation and acute aerobic exercise.
Hwang J1, Castelli DM1, Gonzalez-Lima F2.
Author information
Abstract
This is the first randomized, controlled study comparing the cognitive effects of transcranial laser stimulation and acute aerobic exercise on the same cognitive tasks. We examined whether transcranial infrared laser stimulation of the prefrontal cortex, acute high-intensity aerobic exercise, or the combination may enhance performance in sustained attention and working memory tasks. Sixty healthy young adults were randomly assigned to one of the following four treatments: (1) low-level laser therapy (LLLT) with infrared laser to two forehead sites while seated (total 8 min, 1064 nm continuous wave, 250 mW/cm2, 60 J/cm2 per site of 13.6 cm2); (2) acute exercise (EX) of high-intensity (total 20 min, with 10-min treadmill running at 85-90 % VO2max); (3) combined treatment (LLLT + EX); or (4) sham control (CON). Participants were tested for prefrontal measures of sustained attention with the psychomotor vigilance task (PVT) and working memory with the delayed match-to-sample task (DMS) before and after the treatments. As compared to CON, both LLLT and EX reduced reaction time in the PVT [F(1.56) = 4.134, p = 0.01, η 2 = 0.181] and increased the number of correct responses in the DMS [F(1.56) = 4.690, p = 0.005, η 2 = 0.201], demonstrating a significant enhancing effect of LLLT and EX on cognitive performance. LLLT + EX effects were similar but showed no significantly greater improvement on PVT and DMS than LLLT or EX alone. The transcranial infrared laser stimulation and acute aerobic exercise treatments were similarly effective for cognitive enhancement, suggesting that they augment prefrontal cognitive functions similarly.
https://www.ncbi.nlm.nih.gov/pubmed/27080072
Restor Neurol Neurosci. 2016 Apr 11. [Epub ahead of print]
Non-invasive brain stimulation to promote alertness and awareness in chronic patients with disorders of consciousness: Low-level, near-infrared laser stimulation vs. focused shock wave therapy.
Werner C1, Byhahn M2, Hesse S1.
Author information
Abstract
PURPOSE:
In order to promote alertness and awareness in patients with severe disorders of consciousness (DOC) frontal near infrared laser stimulation (N-LT) or transcranial focused shock wave therapy (F-SWT) might be an option. The study compared both techniques in severe chronic DOC patients.
METHODS:
Sixteen DOC patients were allocated to two groups (A and B). A three week baseline either followed a frontal N-LT (0,1 mJ/mm2, 10 min per session), five times a week over four weeks (group A), or a F-SWT (0,1 mJ/mm2, 4000 stimuli per session) three times a week over four weeks (group B). The primary variable was the revised Coma Recovery Scale (r-CRS, 0-23), blindly assessed.
RESULTS:
Both groups improved in the r-CRS over time, but revealed no differences between groups. One patient of group B had a focal seizure in the third therapy week. One patient with akinetic mutism improved most and three patients with global hypoxia did not improve at all.
CONCLUSIONS:
Both options might be an option to increase alertness and awareness of chronic DOC patients. An akinetic mutism seems to be a positive and severe cerebral hypoxia a negative predictor. Epileptic seizures are a potential unwanted side effect. More clinical studies are warranted.
https://www.ncbi.nlm.nih.gov/pubmed/26817446
Lasers Surg Med. 2016 Apr;48(4):343-9. doi: 10.1002/lsm.22471. Epub 2016 Jan 12.
Transcranial laser stimulation improves human cerebral oxygenation.
Tian F1, Hase SN1, Gonzalez-Lima F2, Liu H1.
Author information
Abstract
BACKGROUND AND OBJECTIVE:
Transcranial laser stimulation of the brain with near-infrared light is a novel form of non-invasive photobiomodulation or low-level laser therapy (LLLT) that has shown therapeutic potential in a variety of neurological and psychological conditions. Understanding of its neurophysiological effects is essential for mechanistic study and treatment evaluation. This study investigated how transcranial laser stimulation influences cerebral hemodynamics and oxygenation in the human brain in vivo using functional near-infrared spectroscopy (fNIRS).
MATERIALS AND METHODS:
Two separate experiments were conducted in which 1,064-nm laser stimulation was administered at (1) the center and (2) the right side of the forehead, respectively. The laser emitted at a power of 3.4 W and in an area of 13.6 cm(2) , corresponding to 0.25 W/cm(2) irradiance. Stimulation duration was 10 minutes. Nine healthy male and female human participants of any ethnic background, in an age range of 18-40 years old were included in each experiment.
RESULTS:
In both experiments, transcranial laser stimulation induced an increase of oxygenated hemoglobin concentration (Δ[HbO2 ]) and a decrease of deoxygenated hemoglobin concentration (Δ[Hb]) in both cerebral hemispheres. Improvements in cerebral oxygenation were indicated by a significant increase of differential hemoglobin concentration (Δ[HbD] = Δ[HbO2 ] - Δ[Hb]). These effects increased in a dose-dependent manner over time during laser stimulation (10 minutes) and persisted after laser stimulation (6 minutes). The total hemoglobin concentration (Δ[HbT] = Δ[HbO2] + Δ[Hb]) remained nearly unchanged in most cases.
CONCLUSION:
Near-infrared laser stimulation applied to the forehead can transcranially improve cerebral oxygenation in healthy humans.
https://www.ncbi.nlm.nih.gov/pubmed/26535475
Adv Mind Body Med. 2015 Fall;29(4):27-33.
SPECT Perfusion Imaging Demonstrates Improvement of Traumatic Brain Injury With Transcranial Near-infrared Laser Phototherapy.
Henderson TA, Morries LD.
Abstract
Traumatic brain injury (TBI) is a growing health concern affecting civilians and military personnel. Near-infrared (NIR) light has shown benefits in animal models and human trials for stroke and in animal models for TBI. Diodes emitting low-level NIR often have lacked therapeutic efficacy, perhaps failing to deliver sufficient radiant energy to the necessary depth. In this case report, a patient with moderate TBI documented in anatomical magnetic resonance imaging (MRI) and perfusion single-photon emission computed tomography (SPECT) received 20 NIR treatments in the course of 2 mo using a high-power NIR laser. Symptoms were monitored by clinical examination and a novel patient diary system specifically designed for this patient population. Clinical application of these levels of infrared energy for this patient with TBI yielded highly favorable outcomes with decreased depression, anxiety, headache, and insomnia, whereas cognition and quality of life improved. Neurological function appeared to improve based on changes in the SPECT by quantitative analysis. NIR in the power range of 10-15 W at 810 and 980 nm can safely and effectively treat chronic symptoms of TBI.
https://www.ncbi.nlm.nih.gov/pubmed/26347062
Neuropsychiatr Dis Treat. 2015 Aug 20;11:2159-75. doi: 10.2147/NDT.S65809. eCollection 2015.
Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy.
Morries LD1, Cassano P2, Henderson TA3.
Author information
Abstract
Traumatic brain injury (TBI) is a growing health concern affecting civilians and military personnel. In this review, treatments for the chronic TBI patient are discussed, including pharmaceuticals, nutraceuticals, cognitive therapy, and hyperbaric oxygen therapy. All available literature suggests a marginal benefit with prolonged treatment courses. An emerging modality of treatment is near-infrared (NIR) light, which has benefit in animal models of stroke, spinal cord injury, optic nerve injury, and TBI, and in human trials for stroke and TBI. The extant literature is confounded by variable degrees of efficacy and a bewildering array of treatment parameters. Some data indicate that diodes emitting low-level NIR energy often have failed to demonstrate therapeutic efficacy, perhaps due to failing to deliver sufficient radiant energy to the necessary depth. As part of this review, we present a retrospective case series using high-power NIR laser phototherapy with a Class IV laser to treat TBI. We demonstrate greater clinical efficacy with higher fluence, in contrast to the bimodal model of efficacy previously proposed. In ten patients with chronic TBI (average time since injury 9.3 years) given ten treatments over the course of 2 months using a high-power NIR laser (13.2 W/0.89 cm(2) at 810 nm or 9 W/0.89 cm(2) at 810 nm and 980 nm), symptoms of headache, sleep disturbance, cognition, mood dysregulation, anxiety, and irritability improved. Symptoms were monitored by depression scales and a novel patient diary system specifically designed for this study. NIR light in the power range of 10-15 W at 810 nm and 980 nm can safely and effectively treat chronic symptoms of TBI. The clinical benefit and effects of infrared phototherapy on mitochondrial function and secondary molecular events are discussed in the context of adequate radiant energy penetration.
https://www.ncbi.nlm.nih.gov/pubmed/26017772
J Neuropsychol. 2015 May 28. doi: 10.1111/jnp.12074. [Epub ahead of print]
Improving executive function using transcranial infrared laser stimulation.
Blanco NJ1,2, Maddox WT1,2,3,4, Gonzalez-Lima F1,3,5.
Author information
Abstract
Transcranial infrared laser stimulation is a new non-invasive form of low-level light therapy that may have a wide range of neuropsychological applications. It entails using low-power and high-energy-density infrared light from lasers to increase metabolic energy. Preclinical work showed that this intervention can increase cortical metabolic energy, thereby improving frontal cortex-based memory function in rats. Barrett and Gonzalez-Lima (2013, Neuroscience, 230, 13) discovered that transcranial laser stimulation can enhance sustained attention and short-term memory in humans. We extend this line of work to executive function. Specifically, we ask whether transcranial laser stimulation enhances performance in the Wisconsin Card Sorting Task that is considered the gold standard of executive function and is compromised in normal ageing and a number of neuropsychological disorders. We used a laser of a specific wavelength (1,064 nm) that photostimulates cytochrome oxidase – the enzyme catalysing oxygen consumption for metabolic energy production. Increased cytochrome oxidase activity is considered the primary mechanism of action of this intervention. Participants who received laser treatment made fewer errors and showed improved set-shifting ability relative to placebo controls. These results suggest that transcranial laser stimulation improves executive function and may have exciting potential for treating or preventing deficits resulting from neuropsychological disorders or normal ageing.
https://www.ncbi.nlm.nih.gov/pubmed/25277249
Lasers Med Sci. 2015 Jan;30(1):339-46. doi: 10.1007/s10103-014-1669-2. Epub 2014 Oct 3.
The effects of transcranial LED therapy (TCLT) on cerebral blood flow in the elderly women.
Salgado AS1, Zângaro RA, Parreira RB, Kerppers II.
Author information
Abstract
During aging processes, there is a range of functional changes, where we can highlight the disease related to the central nervous system, such as Alzheimer disease and others forms of dementia. This study investigated the effects of transcranial light emitting diode (LED) on cerebral blood flow in healthy elderly women analyzed by transcranial Doppler ultrasound (TCD) of the right and left middle cerebral artery and basilar artery. Twenty-five noninstitutionalized elderly women (mean age 72 years old), with a cognitive status >24, were assessed using transcranial Doppler ultrasound on two separate occasions: pre-irradiation and post-transcranial LED therapy (TCLT). Prior to this, they answered two questionnaires: the perceived stress scale and the general health questionnaire. TCLT (627 nm, 70 mW/cm(2), 10 J/cm(2)) was performed at four points of the frontal and parietal region for 30 s each, totaling 120 s two times per week for 4 weeks. Paired t-test results showed that there was a significant improvement after TCLT with increase in the systolic and diastolic velocity of the left middle cerebral artery (25 and 30%, respectively) and basilar artery (up to 17 and 25%), as well as a decrease in the pulsatility index and resistance index values of the three cerebral arteries analyzed (p < 0.05). TCD parameters showed improvement in the blood flow on the arteries analyzed. TCLT promoted a blood and vasomotor behavior of the basilar and middle cerebral arteries in healthy elderly women.
https://www.ncbi.nlm.nih.gov/pubmed/24568233
J Neurotrauma. 2014 Jun 1;31(11):1008-17. doi: 10.1089/neu.2013.3244. Epub 2014 May 8.
Significant improvements in cognitive performance post-transcranial, red/near-infrared light-emitting diode treatments in chronic, mild traumatic brain injury: open-protocol study.
Naeser MA1, Zafonte R, Krengel MH, Martin PI, Frazier J, Hamblin MR, Knight JA, Meehan WP 3rd, Baker EH.
Author information
Abstract
This pilot, open-protocol study examined whether scalp application of red and near-infrared (NIR) light-emitting diodes (LED) could improve cognition in patients with chronic, mild traumatic brain injury (mTBI). Application of red/NIR light improves mitochondrial function (especially in hypoxic/compromised cells) promoting increased adenosine triphosphate (ATP) important for cellular metabolism. Nitric oxide is released locally, increasing regional cerebral blood flow. LED therapy is noninvasive, painless, and non-thermal (cleared by the United States Food and Drug Administration [FDA], an insignificant risk device). Eleven chronic, mTBI participants (26-62 years of age, 6 males) with nonpenetrating brain injury and persistent cognitive dysfunction were treated for 18 outpatient sessions (Monday, Wednesday, Friday, for 6 weeks), starting at 10 months to 8 years post- mTBI (motor vehicle accident [MVA] or sports-related; and one participant, improvised explosive device [IED] blast injury). Four had a history of multiple concussions. Each LED cluster head (5.35 cm diameter, 500 mW, 22.2 mW/cm(2)) was applied for 10 min to each of 11 scalp placements (13 J/cm(2)). LEDs were placed on the midline from front-to-back hairline; and bilaterally on frontal, parietal, and temporal areas. Neuropsychological testing was performed pre-LED, and at 1 week, and 1 and 2 months after the 18th treatment. A significant linear trend was observed for the effect of LED treatment over time for the Stroop test for Executive Function, Trial 3 inhibition (p=0.004); Stroop, Trial 4 inhibition switching (p=0.003); California Verbal Learning Test (CVLT)-II, Total Trials 1-5 (p=0.003); and CVLT-II, Long Delay Free Recall (p=0.006). Participants reported improved sleep, and fewer post-traumatic stress disorder (PTSD) symptoms, if present. Participants and family reported better ability to perform social, interpersonal, and occupational functions. These open-protocol data suggest that placebo-controlled studies are warranted.
https://www.ncbi.nlm.nih.gov/pubmed/24136303
Lasers Surg Med. 2013 Dec;45(10):648-53. doi: 10.1002/lsm.22190. Epub 2013 Oct 17.
Transcranial application of near-infrared low-level laser can modulate cortical excitability.
Konstantinović LM1, Jelić MB, Jeremić A, Stevanović VB, Milanović SD, Filipović SR.
Author information
Abstract
BACKGROUND AND OBJECTIVE:
Near-infrared low-level laser (NIR-LLL) irradiation penetrates scalp and skull and can reach superficial layers of the cerebral cortex. It was shown to improve the outcome of acute stroke in both animal and human studies. In this study we evaluated whether transcranial laser stimulation (TLS) with NIR-LLL can modulate the excitability of the motor cortex (M1) as measured by transcranial magnetic stimulation (TMS).
METHODS:
TLS was applied for 5 minutes over the representation of the right first dorsal interosseal muscle (FDI) in left primary motor cortex (M1), in 14 healthy subjects. Motor evoked potentials (MEPs) from the FDI, elicited by single-pulse TMS, were measured at baseline and up to 30 minutes after the TLS.
RESULTS:
The average MEP size was significantly reduced during the first 20 minutes following the TLS. The pattern was present in 10 (71.5%) of the participants. The MEP size reduction correlated negatively with the motor threshold at rest.
CONCLUSIONS:
TLS with NIR-LLL induced transitory reduction of the excitability of the stimulated cortex. These findings give further insights into the mechanisms of TLS effects in the human cerebral cortex, paving the way for potential applications of TLS in treatment of stroke and in other clinical settings.
https://www.ncbi.nlm.nih.gov/pubmed/23200785
Neuroscience. 2013 Jan 29;230:13-23. doi: 10.1016/j.neuroscience.2012.11.016. Epub 2012 Nov 27.
Transcranial infrared laser stimulation produces beneficial cognitive and emotional effects in humans.
Barrett DW1, Gonzalez-Lima F.
Author information
Abstract
This is the first controlled study demonstrating the beneficial effects of transcranial laser stimulation on cognitive and emotional functions in humans. Photobiomodulation with red to near-infrared light is a novel intervention shown to regulate neuronal function in cell cultures, animal models, and clinical conditions. Light that intersects with the absorption spectrum of cytochrome oxidase was applied to the forehead of healthy volunteers using the laser diode CG-5000, which maximizes tissue penetration and has been used in humans for other indications. We tested whether low-level laser stimulation produces beneficial effects on frontal cortex measures of attention, memory and mood. Reaction time in a sustained-attention psychomotor vigilance task (PVT) was significantly improved in the treated (n=20) vs. placebo control (n=20) groups, especially in high novelty-seeking subjects. Performance in a delayed match-to-sample (DMS) memory task showed also a significant improvement in treated vs. control groups as measured by memory retrieval latency and number of correct trials. The Positive and Negative Affect Schedule (PANAS-X), which tracks self-reported positive and negative affective (emotional) states over time, was administered immediately before treatment and 2 weeks after treatment. The PANAS showed that while participants generally reported more positive affective states than negative, overall affect improved significantly in the treated group due to more sustained positive emotional states as compared to the placebo control group. These data imply that transcranial laser stimulation could be used as a non-invasive and efficacious approach to increase brain functions such as those related to cognitive and emotional dimensions. Transcranial infrared laser stimulation has also been proven to be safe and successful at improving neurological outcome in humans in controlled clinical trials of stroke. This innovative approach could lead to the development of non-invasive, performance-enhancing interventions in healthy humans and in those in need of neuropsychological rehabilitation.
https://www.ncbi.nlm.nih.gov/pubmed/21182447
Photomed Laser Surg. 2011 May;29(5):351-8. doi: 10.1089/pho.2010.2814. Epub 2010 Dec 23.
Improved cognitive function after transcranial, light-emitting diode treatments in chronic, traumatic brain injury: two case reports.
Naeser MA1, Saltmarche A, Krengel MH, Hamblin MR, Knight JA.
Author information
Abstract
OBJECTIVE:
Two chronic, traumatic brain injury (TBI) cases, where cognition improved following treatment with red and near-infrared light-emitting diodes (LEDs), applied transcranially to forehead and scalp areas, are presented.
BACKGROUND:
Significant benefits have been reported following application of transcranial, low-level laser therapy (LLLT) to humans with acute stroke and mice with acute TBI. These are the first case reports documenting improved cognitive function in chronic, TBI patients treated with transcranial LED.
METHODS:
Treatments were applied bilaterally and to midline sagittal areas using LED cluster heads [2.1″ diameter, 61 diodes (9 × 633 nm, 52 × 870 nm); 12-15 mW per diode; total power: 500 mW; 22.2 mW/cm(2); 13.3 J/cm(2) at scalp (estimated 0.4 J/cm(2) to cortex)].
RESULTS:
Seven years after closed-head TBI from a motor vehicle accident, Patient 1 began transcranial LED treatments. Pre-LED, her ability for sustained attention (computer work) lasted 20 min. After eight weekly LED treatments, her sustained attention time increased to 3 h. The patient performs nightly home treatments (5 years); if she stops treating for more than 2 weeks, she regresses. Patient 2 had a history of closed-head trauma (sports/military, and recent fall), and magnetic resonance imaging showed frontoparietal atrophy. Pre-LED, she was on medical disability for 5 months. After 4 months of nightly LED treatments at home, medical disability discontinued; she returned to working full-time as an executive consultant with an international technology consulting firm. Neuropsychological testing after 9 months of transcranial LED indicated significant improvement (+1, +2SD) in executive function (inhibition, inhibition accuracy) and memory, as well as reduction in post-traumatic stress disorder. If she stops treating for more than 1 week, she regresses. At the time of this report, both patients are continuing treatment.
CONCLUSIONS:
Transcranial LED may improve cognition, reduce costs in TBI treatment, and be applied at home. Controlled studies are warranted.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2796659/
Behav Brain Funct. 2009; 5: 46.
Published online 2009 Dec 8. doi: 10.1186/1744-9081-5-46
PMCID: PMC2796659
Psychological benefits 2 and 4 weeks after a single treatment with near infrared light to the forehead: a pilot study of 10 patients with major depression and anxiety
Fredric Schiffer,corresponding author1 Andrea L Johnston,3 Caitlin Ravichandran,2 Ann Polcari,1 Martin H Teicher,1 Robert H Webb,3,4 and Michael R Hamblin3,4,5
Abstract
Background
Many studies have reported beneficial effects from the application of near-infrared (NIR) light photobiomodulation (PBM) to the body, and one group has reported beneficial effects applying it to the brain in stroke patients. We have reported that the measurement of a patient’s left and right hemispheric emotional valence (HEV) may clarify data and guide lateralized treatments. We sought to test whether a NIR treatment could 1. improve the psychological status of patients, 2. show a relationship between immediate psychological improvements when HEV was taken into account, and 3. show an increase in frontal pole regional cerebral blood flow (rCBF), and 4. be applied without side effects.
Methods
We gave 10 patients, (5 M/5 F) with major depression, including 9 with anxiety, 7 with a past history of substance abuse (6 with an opiate abuse and 1 with an alcohol abuse history), and 3 with post traumatic stress disorder, a baseline standard diagnostic interview, a Hamilton Depression Rating Scale (HAM-D), a Hamilton Anxiety Rating Scale (HAM-A), and a Positive and Negative Affect Scale (PANAS). We then gave four 4-minute treatments in a random order: NIR to left forehead at F3, to right forehead at F4, and placebo treatments (light off) at the same sites. Immediately following each treatment we repeated the PANAS, and at 2-weeks and at 4-weeks post treatment we repeated all 3 rating scales. During all treatments we recorded total hemoglobin (cHb), as a measure of rCBF with a commercial NIR spectroscopy device over the left and the right frontal poles of the brain.
Results
At 2-weeks post treatment 6 of 10 patients had a remission (a score ≤ 10) on the HAM-D and 7 of 10 achieved this on the HAM-A. Patients experienced highly significant reductions in both HAM-D and HAM-A scores following treatment, with the greatest reductions occurring at 2 weeks. Mean rCBF across hemispheres increased from 0.011 units in the off condition to 0.043 units in the on condition, for a difference of 0.032 (95% CI: -0.016, 0.080) units, though this result did not reach statistical significance. Immediately after treatment the PANAS improved to a significantly greater extent with NIR “on” relative to NIR “off” when a hemisphere with more positive HEV was treated than when one with more negative HEV was treated. We observed no side effects.
Conclusion
This small feasibility study suggests that NIR-PBM may have utility for the treatment of depression and other psychiatric disorders and that double blind randomized placebo-controlled trials are indicated.
https://www.ncbi.nlm.nih.gov/pubmed/19233936
Stroke. 2009 Apr;40(4):1359-64. doi: 10.1161/STROKEAHA.109.547547. Epub 2009 Feb 20.
Effectiveness and safety of transcranial laser therapy for acute ischemic stroke.
Zivin JA1, Albers GW, Bornstein N, Chippendale T, Dahlof B, Devlin T, Fisher M, Hacke W, Holt W, Ilic S, Kasner S, Lew R, Nash M, Perez J, Rymer M, Schellinger P, Schneider D, Schwab S, Veltkamp R, Walker M, Streeter J; NeuroThera Effectiveness and Safety Trial-2 Investigators.
Author information
Abstract
BACKGROUND AND PURPOSE:
We hypothesized that transcranial laser therapy (TLT) can use near-infrared laser technology to treat acute ischemic stroke. The NeuroThera Effectiveness and Safety Trial-2 (NEST-2) tested the safety and efficacy of TLT in acute ischemic stroke.
METHODS:
This double-blind, randomized study compared TLT treatment to sham control. Patients receiving tissue plasminogen activator and patients with evidence of hemorrhagic infarct were excluded. The primary efficacy end point was a favorable 90-day score of 0 to 2 assessed by the modified Rankin Scale. Other 90-day end points included the overall shift in modified Rankin Scale and assessments of change in the National Institutes of Health Stroke Scale score.
RESULTS:
We randomized 660 patients: 331 received TLT and 327 received sham; 120 (36.3%) in the TLT group achieved favorable outcome versus 101 (30.9%), in the sham group (P=0.094), odds ratio 1.38 (95% CI, 0.95 to 2.00). Comparable results were seen for the other outcome measures. Although no prespecified test achieved significance, a post hoc analysis of patients with a baseline National Institutes of Health Stroke Scale score of <16 showed a favorable outcome at 90 days on the primary end point (P<0.044). Mortality rates and serious adverse events did not differ between groups with 17.5% and 17.4% mortality, 37.8% and 41.8% serious adverse events for TLT and sham, respectively.
CONCLUSIONS:
TLT within 24 hours from stroke onset demonstrated safety but did not meet formal statistical significance for efficacy. However, all predefined analyses showed a favorable trend, consistent with the previous clinical trial (NEST-1). Both studies indicate that mortality and adverse event rates were not adversely affected by TLT. A definitive trial with refined baseline National Institutes of Health Stroke Scale exclusion criteria is planned.
https://www.ncbi.nlm.nih.gov/pubmed/17463313
Stroke. 2007 Jun;38(6):1843-9. Epub 2007 Apr 26.
Infrared laser therapy for ischemic stroke: a new treatment strategy: results of the NeuroThera Effectiveness and Safety Trial-1 (NEST-1).
Lampl Y1, Zivin JA, Fisher M, Lew R, Welin L, Dahlof B, Borenstein P, Andersson B, Perez J, Caparo C, Ilic S, Oron U.
Author information
Abstract
BACKGROUND AND PURPOSE:
The NeuroThera Effectiveness and Safety Trial-1 (NEST-1) study evaluated the safety and preliminary effectiveness of the NeuroThera Laser System in the ability to improve 90-day outcomes in ischemic stroke patients treated within 24 hours from stroke onset. The NeuroThera Laser System therapeutic approach involves use of infrared laser technology and has shown significant and sustained beneficial effects in animal models of ischemic stroke.
METHODS:
This was a prospective, intention-to-treat, multicenter, international, double-blind, trial involving 120 ischemic stroke patients treated, randomized 2:1 ratio, with 79 patients in the active treatment group and 41 in the sham (placebo) control group. Only patients with baseline stroke severity measured by National Institutes of Health Stroke Scale (NIHSS) scores of 7 to 22 were included. Patients who received tissue plasminogen activator were excluded. Outcome measures were the patients’ scores on the NIHSS, modified Rankin Scale (mRS), Barthel Index, and Glasgow Outcome Scale at 90 days after treatment. The primary outcome measure, prospectively identified, was successful treatment, documented by NIHSS. This was defined as a complete recovery at day 90 (NIHSS 0 to 1), or a decrease in NIHSS score of at least 9 points (day 90 versus baseline), and was tested as a binary measure (bNIH). Secondary outcome measures included mRS, Barthel Index, and Glasgow Outcome Scale. Primary statistical analyses were performed with the Cochran-Mantel-Haenszel rank test, stratified by baseline NIHSS score or by time to treatment for the bNIH and mRS. Logistic regression analyses were conducted to confirm the results.
RESULTS:
Mean time to treatment was >16 hours (median time to treatment 18 hours for active and 17 hours for control). Time to treatment ranged from 2 to 24 hours. More patients (70%) in the active treatment group had successful outcomes than did controls (51%), as measured prospectively on the bNIH (P=0.035 stratified by severity and time to treatment; P=0.048 stratified only by severity). Similarly, more patients (59%) had successful outcomes than did controls (44%) as measured at 90 days as a binary mRS score of 0 to 2 (P=0.034 stratified by severity and time to treatment; P=0.043 stratified only by severity). Also, more patients in the active treatment group had successful outcomes than controls as measured by the change in mean NIHSS score from baseline to 90 days (P=0.021 stratified by time to treatment) and the full mRS (“shift in Rankin”) score (P=0.020 stratified by severity and time to treatment; P=0.026 stratified only by severity). The prevalence odds ratio for bNIH was 1.40 (95% CI, 1.01 to 1.93) and for binary mRS was 1.38 (95% CI, 1.03 to 1.83), controlling for baseline severity. Similar results held for the Barthel Index and Glasgow Outcome Scale. Mortality rates and serious adverse events (SAEs) did not differ significantly (8.9% and 25.3% for active 9.8% and 36.6% for control, respectively, for mortality and SAEs).
CONCLUSIONS:
The NEST-1 study indicates that infrared laser therapy has shown initial safety and effectiveness for the treatment of ischemic stroke in humans when initiated within 24 hours of stroke onset. A larger confirmatory trial to demonstrate safety and effectiveness is warranted.

4 Comments
Leave your reply.